Critical Thinking in Healthcare: Evaluating Medical Advice
Written on
Chapter 1: The Importance of Critical Evaluation
In today's world, where evidence-based medicine is paramount, it’s essential to approach medical guidance with a critical mindset. Empirical evidence is the cornerstone of understanding our reality; claims without strong backing are often untrustworthy.
It's crucial to remember that assertions and beliefs hold no value unless validated by consistent, reproducible evidence.
Section 1.1: The Shortcomings of Conventional Medicine
Despite advancements, many aspects of medical practice still rely on outdated beliefs rather than empirical data. This is particularly evident in regions where superstition prevails over scientific understanding. Practices such as witchcraft for healing are not uncommon in certain cultures, while in the West, some individuals still hold on to unscientific remedies like crystals and essential oils.
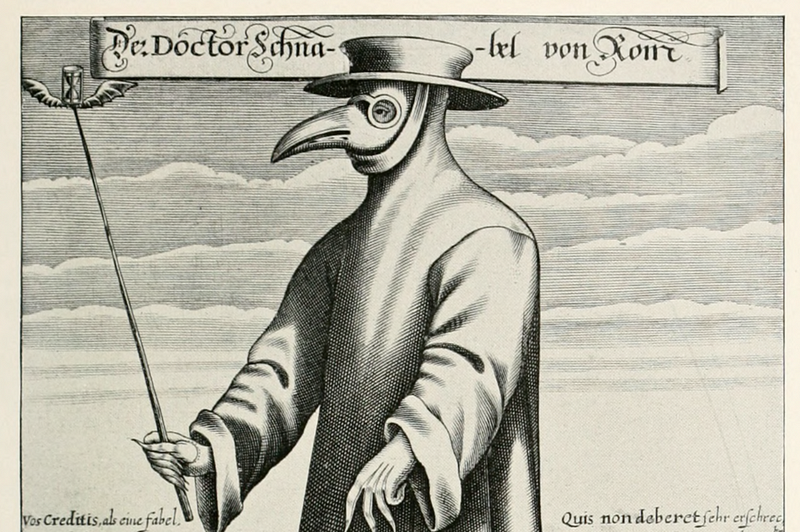
Section 1.2: Historical Missteps in Medical Advice
Historically, numerous medical recommendations have been misguided. For instance, the practice of lying on one’s back during childbirth was adopted more for the convenience of practitioners than for the well-being of the patient, leading to unnecessary pain during delivery.
It took over a century for medical professionals to reevaluate childbirth methods, and even today, the American healthcare system often prioritizes profit over optimal outcomes. Current cesarean section rates remain around 30%, while evidence suggests they should be between 0.2% and 2%.
Chapter 2: Learning from Past Mistakes
The second video title is "The Finfluencer Conundrum: Not All Advice is Created Equal - YouTube"
Doctors once routinely removed tonsils and adenoids from young patients "as a precaution," despite these organs being critical to the immune system. This practice persists in certain areas, despite clear evidence that such procedures are largely unnecessary and detrimental.
Similarly, throughout the mid-20th century, doctors overprescribed antibiotics, ignoring warnings about the rise of antibiotic-resistant superbugs, which has now become a significant public health issue.
Section 2.1: The Need for Evidence in Medical Practices
Doctors have often recommended spinal fusion for back pain, despite substantial evidence indicating that this approach does not alleviate pain and can worsen the condition.
In the UK, there was a time when dental professionals suggested extracting all teeth by age 21 to avoid future issues, based on the flawed assumption that all teeth would decay.
Just because a medical professional offers advice, it does not mean it is inherently correct. We should not take medical guidance at face value, just as we would critically assess claims made by a used car salesperson.
Section 2.2: The Role of Data in Medical Decision-Making
The burden of evaluating medical claims lies with individuals. With the advent of the Internet, accessing empirical data has become more manageable, enabling informed decision-making.
Reliable conclusions stem from rigorous investigation rather than opinion. For instance, misguided claims about wheat being harmful or vaccines causing autism lack empirical support, and credible data disproves these assertions.
We are fortunate to be in an era where data is gradually refining medical practices, although we have a long journey ahead. Much of current medical advice still hinges on beliefs rather than solid evidence.
As we consume media narratives about health recommendations, it’s wise to remember that past generations were once advised to consume arsenic for health benefits.
In conclusion, developing a habit of reasoning based on facts, rather than succumbing to the allure of immediate action or authority figures, is vital. Our evolutionary heritage has equipped us with basic reasoning skills; it is time to utilize them effectively.